Shortwave IR quantum dots enable highly detailed body imaging
![]()
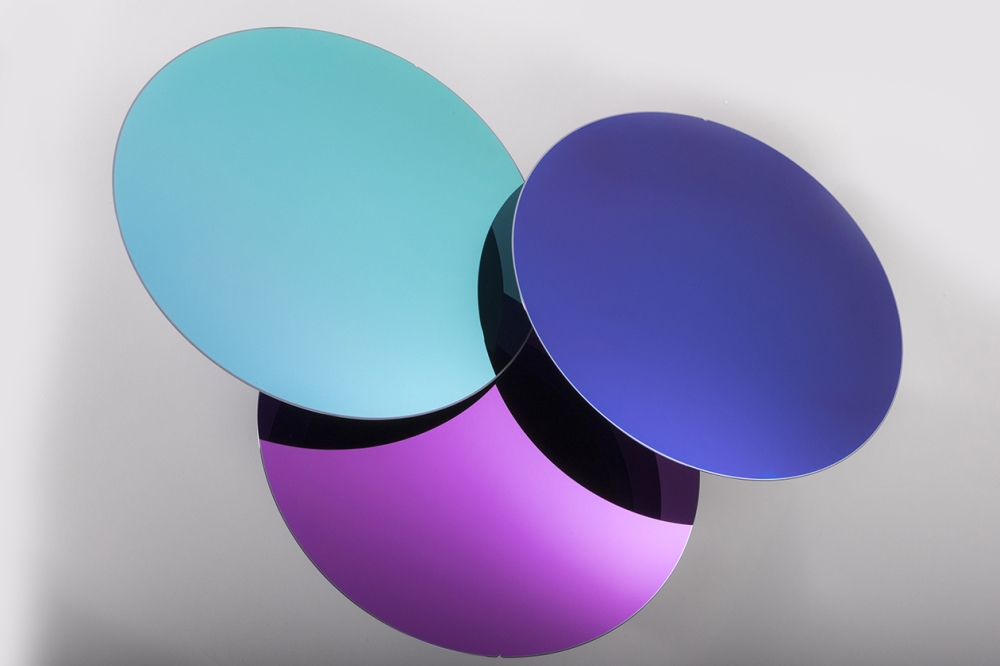
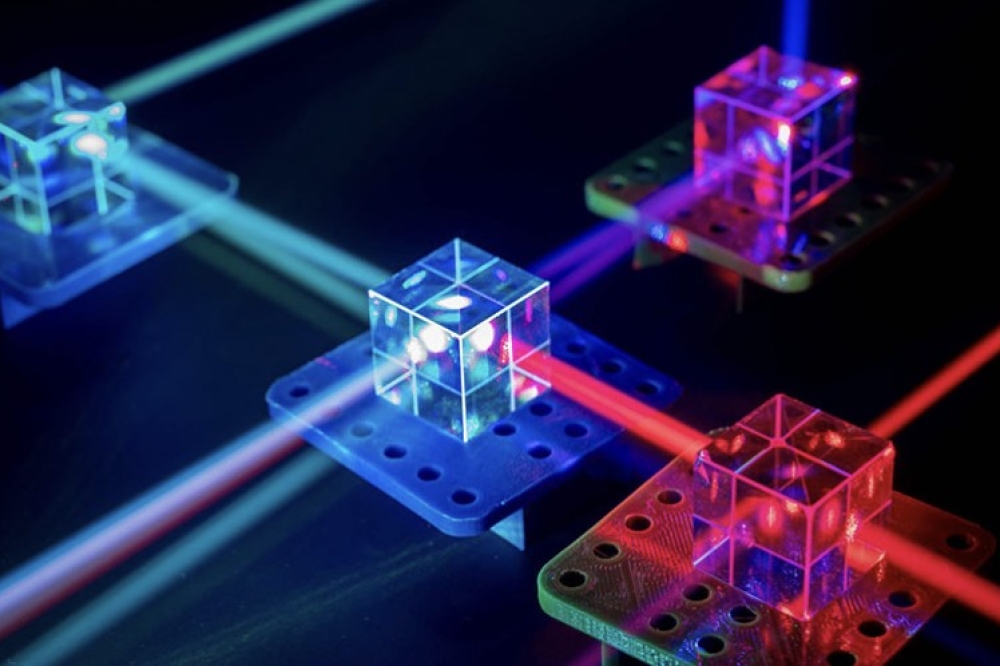
Above: Shortwave IR quantum dots for next generation in vivo optical imaging
Researchers have shown how InAs quantum dots can injected into the body to provide a way new way of making detailed images of internal body structures such as fine networks of blood vessels.
The findings are described in a paper 'Next-generation in vivo optical imaging with short-wave infrared quantum dots' in the journal Nature Biomedical Engineering, by MIT research scientist Oliver Bruns, recent graduate Thomas Bischof, professor of chemistry Moungi Bawendi, and 21 others.
Near-infrared imaging for research on biological tissues, with wavelengths between 700 and 900 nm, is widely used, but wavelengths of around 1,000 to 2,000 nm have the potential to provide even better results, because body tissues are more transparent to that light.
"We knew that this imaging mode would be better" than existing methods, Bruns explains, "but we were lacking high-quality emitters".
Light-emitting particles have been a specialty of Bawendi, the Lester Wolf professor of chemistry, whose lab has over the years has developed new ways of making quantum dots, including ones whose frequency can be precisely tuned by controlling their exact size and composition.
The key was to develop quantum dots whose emissions matched the desired short-wave infrared frequencies and were bright enough to then be easily detected through the surrounding skin and muscle tissues.
The team succeeded in making particles that are "orders of magnitude better than previous materials, and that allow unprecedented detail in biological imaging," Bruns says.
The synthesis of these new particles was initially described in a paper by graduate student Daniel Franke and others from the Bawendi group in Nature Communications last year.
The quantum dots the team produced are so bright that their emissions can be captured with very short exposure times, he says. This makes it possible to produce not just single images but video that captures details of motion, such as the flow of blood, making it possible to distinguish between veins and arteries.
The new light-emitting particles are also the first that are bright enough to allow imaging of internal organs in mice that are awake and moving, as opposed to previous methods that required them to be anesthetized, Bruns says.
Initial applications would be for preclinical research in animals, as the compounds contain some materials that are unlikely to be approved for use in humans. The researchers are also working on developing versions that would be safer for humans.
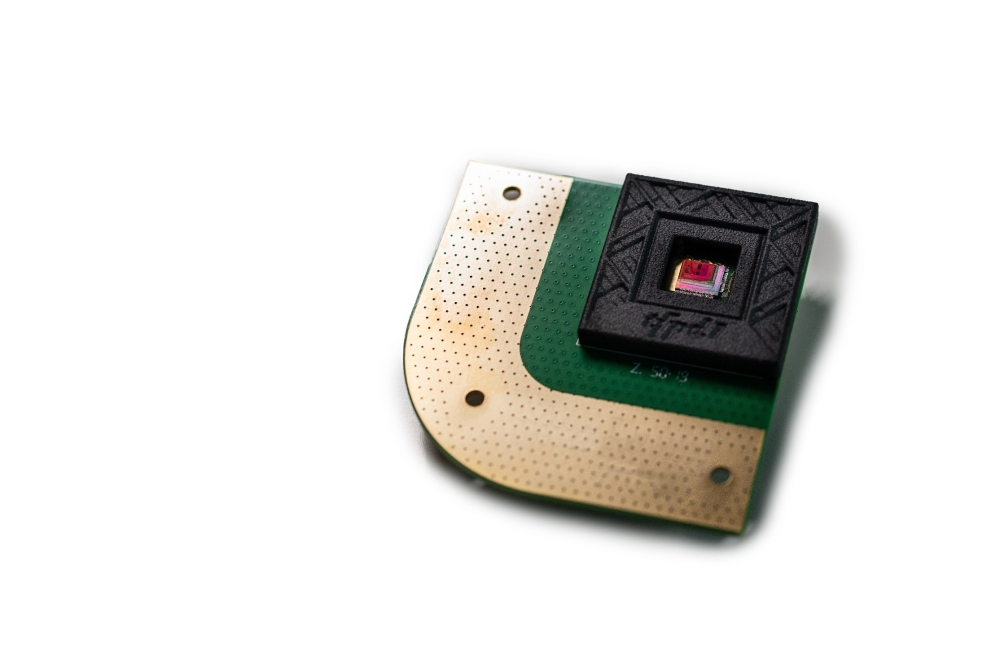
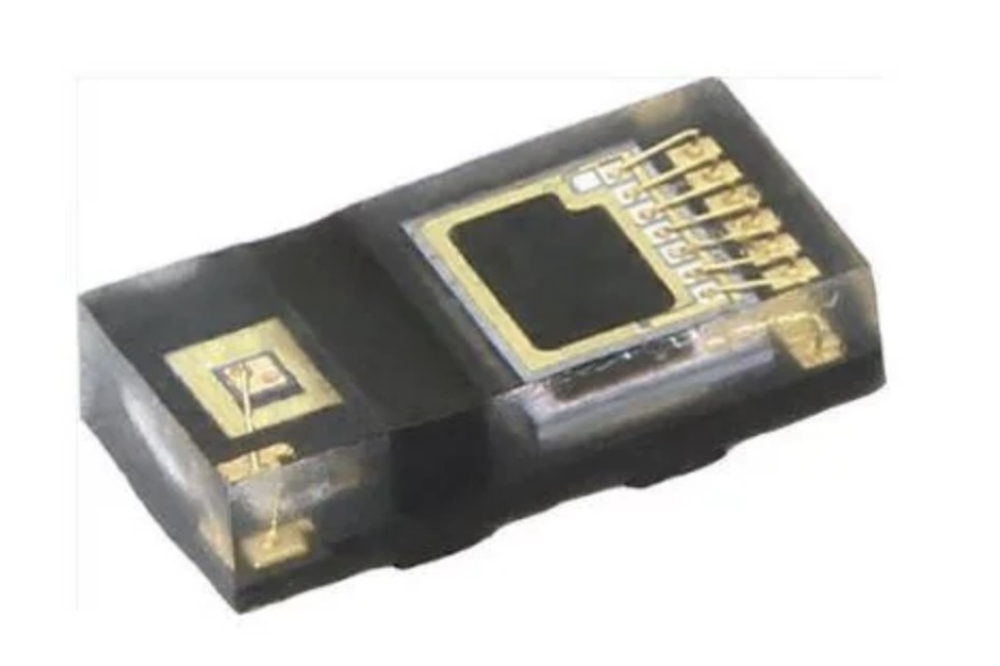
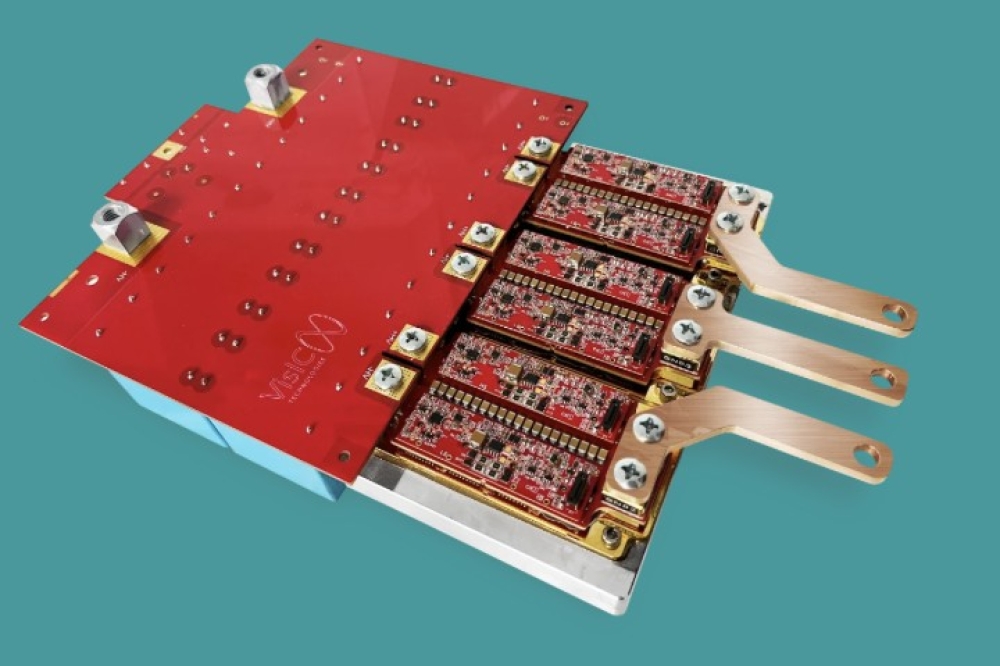
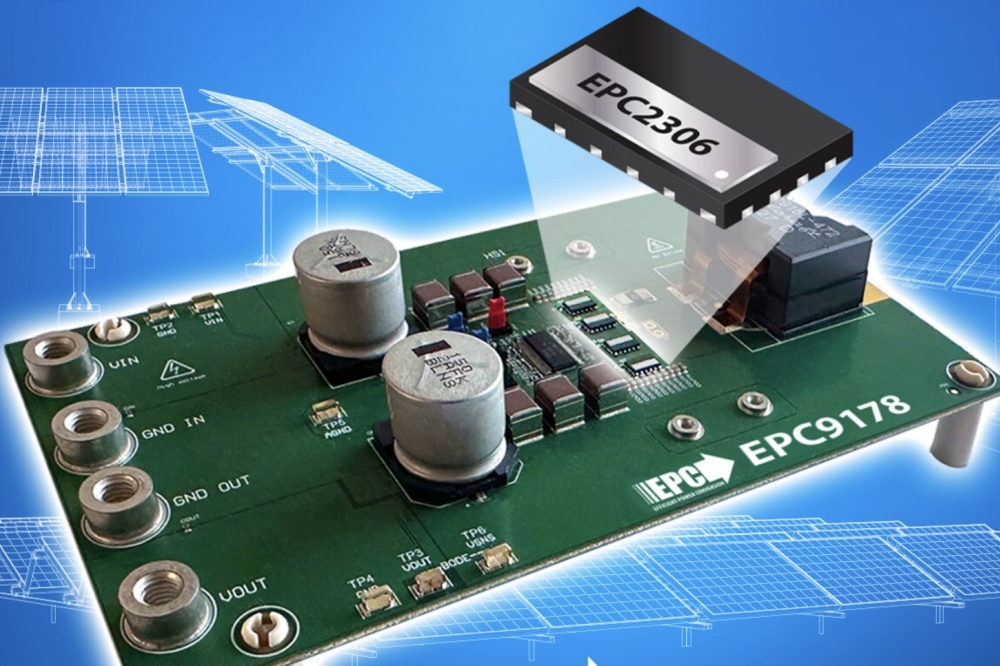
The method also relies on the use of a newly developed camera that is highly sensitive to this particular range of short-wave infrared light. The camera is a commercially developed product, Bruns says, but his team was the first customer for the camera's specialised detector, made of InGaAs. Though this camera was developed for research purposes, these frequencies of infrared light are also used as a way of seeing through fog or smoke.
Not only can the new method determine the direction of blood flow, Bruns says, it is detailed enough to track individual blood cells within that flow. "We can track the flow in each and every capillary, at super high speed," he says. "We can get a quantitative measure of flow, and we can do such flow measurements at very high resolution, over large areas."
Such imaging could potentially be used, for example, to study how the blood flow pattern in a tumour changes as the tumour develops, which might lead to new ways of monitoring disease progression or responsiveness to a drug treatment. "This could give a good indication of how treatments are working that was not possible before," he says.
The team included members from MIT's departments of Chemistry, Chemical Engineering, Biological Engineering, and Mechanical Engineering, as well as from Harvard Medical School, the Harvard T.H. Chan School of Public Health, Raytheon Vision Systems, and University Medical Center in Hamburg, Germany.
The work was supported by the US National Institutes of Health, the National Cancer Institute, the National Foundation for Cancer Research, the Warshaw Institute for Pancreatic Cancer Research, the Massachusetts General Hospital Executive Committee on Research, the US Army Research Office through the Institute for Soldier Nanotechnologies at MIT, the US Department of Defense, and the US National Science Foundation.